
Ankle Dislocation Without Fracture
Mark Tranovich, MD
THE PHYSICIAN AND SPORTSMEDICINE - VOL 31 - NO. 5 - MAY 2003
In Brief: Injuries to the ankle ligaments are common, but injuries severe enough to cause complete tibiotalar dislocation are uncommon. Not all dislocations cause fractures, as seen in the case report of a recreational softball player. Despite the dramatic appearance of the injury, if radiographs do not indicate a fracture and no neurologic or vascular complications are seen, congruent reduction of the ankle can be achieved nonsurgically. After a period of splinting, non-weight bearing, and rehabilitating, most patients make a full recovery.
When a plantar-flexed ankle meets an unyielding inversion force, the stage is set for ligamentous and capsular failure. The result is a dislocated ankle, with or without fracture. Softball and baseball players who slide into rigid bases are particularly at risk for this injury. The following case illustrates why the American Academy of Orthopedic Surgeons encourages the use of breakaway bases to prevent injury.
Case History
A 33-year-old man injured his left ankle while playing recreational softball. He was sliding into an immobile base when his foot caught on it and his momentum carried him over the base.
Physical exam. When the patient was brought to the emergency department, his ankle was deformed, with the entire foot displaced to the medial side (figure 1A). The fibula was prominent laterally, causing tenting of the skin. The dorsalis pedis pulse was still palpable. The patient reported paresthesias, predominantly along the tibial side of the foot to the midfoot and plantar region. Paresthesias on the lateral side of the foot were less pronounced. Sensation was normal above the injury. Capillary refill in his toes was good, and no significant swelling was noted. No lacerations or open wounds were present, and he appeared otherwise healthy.
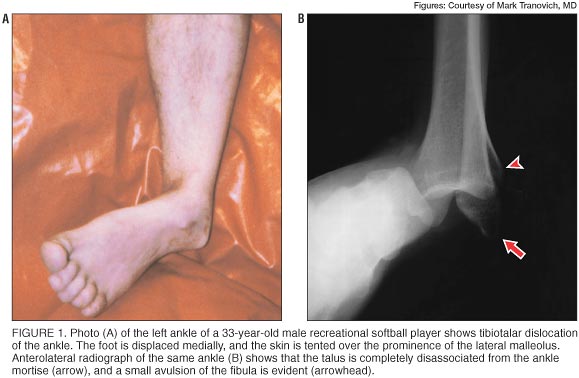
Radiology and diagnosis. Dislocation of the ankle joint and a small avulsion from the distal fibula were seen on standard views of plain radiographs (figure 1B).
Treatment. The clinician easily reduced the dislocation by applying traction with one hand on the heel and other hand on the forefoot. The clinician flexed the patient's knee to relax the gastrocnemius complex and manipulated the ankle. The reduction was apparent, but the paresthesias persisted.
Postreduction radiographs confirmed a concentric reduction (figure 2). After being fitted into a Jones compression dressing and plaster splints, the patient was discharged with instructions to avoid weight bearing until reevaluation.

The paresthesias resolved over the next few weeks. He was taken out of the Jones dressing and placed in a short leg cast at 10 days postinjury. He began weight bearing as tolerated with the cast. When the cast was removed 2 weeks later, ankle range of motion was limited to a few degrees beyond neutral. A functional ankle brace (Aircast Inc, Summit, New Jersey) was prescribed, and the patient underwent 6 weeks of physical therapy to improve his gait and range of motion. At that time he returned to work but not to softball (the season was over). Fourteen months later, he reported no problems with the ankle except for aching with changes in weather. Range of motion was symmetric except that the injured left ankle had 3° less dorsiflexion than the right ankle.
Running Into Trouble
Dislocation of the tibiotalar joint without fracture most commonly occurs in young men and is usually caused by motor vehicle accident, falls, or sports injuries.1-4 Maximum plantar flexion with axial loading and forced inversion of the foot appears to put the ankle at risk of dislocation. The talus has a rhomboidal shape when viewed from the superior aspect, and the posterior portion is narrower than the anterior portion. Plantar flexion places the narrowest portion of the talus in the mortise, the most unstable position. An inversion force then causes ligamentous and capsular failure and the potential for ankle dislocation with or without fracture.2,5,6
In this case, the patient caught his foot while sliding into a fixed base during a softball game. The American Academy of Orthopedic Surgeons has issued a position statement6 endorsing breakaway bases to prevent recreational baseball and softball injuries. Bases that yield to impact reduce the number of sliding injuries.
The standard radiographic studies were sufficient to make the diagnosis, and the success of the closed reduction was demonstrated on repeat radiographs. If the closed reduction had failed, an open reduction would have been required.
The patient refrained from weight bearing while in the Jones dressing because of its bulkiness. He could bear weight in the cast. Since this is an uncommon injury, no "standard" treatment protocol exists. Length of rehabilitation and time before returning to sport will be determined on an individual basis. Data on long-term sequelae, such as instability or degenerative changes, is not available.
Breaking Away
Dislocation of the ankle without fracture is rare. Plain radiographs will confirm the obvious clinical assessment and reveal any avulsions or fractures.
The goal of treatment is to obtain congruent reduction of the ankle. The reduction should be done emergently to prevent further compromise of the skin and neurologic or vascular structures. The neurologic and vascular exam should be documented before and after reduction, and closed reduction should be verified with repeat radiographs. Non-weight bearing is recommended initially, but patients can begin walking as tolerated. Patients who have closed tibiotalar dislocations treated nonoperatively often do well, with little long-term pain, instability, or loss of motion.2-4,7
References
- Holmer P, Sondergaard L, Konradsen L, et al: Epidemiology of sprains in the lateral ankle and foot. Foot Ankle Int 1994;15(2):72-74
- Colville MR, Colville JM, Manoli A II: Posteromedial dislocation of the ankle without fracture. J Bone Joint Surg Am 1987;69(5):706-711
- Moehring HD, Tan RT, Marder RA, et al: Ankle dislocation. J Orthop Trauma 1994;8(2):167-172
- Wroble RR, Nepola JV, Malvitz TA: Ankle dislocation without fracture. Foot Ankle 1988;9(2):64-74
- Fernandes TJ: The mechanism of talo-tibial dislocation without fracture: Proceedings and Reports of Universities, Colleges, Councils, and Associations. J Bone Joint Surg Br 1976;58(3):364-365
- American Academy of Orthopedic Surgeons: Position statement: use of breakaway bases in preventing recreational baseball and softball injuries. Available at http://www.aaos.org/wordhtml/papers/position/bases.htm. Accessed January 17, 2003
- Toohey JS, Worsing RA Jr: The long-term follow-up study of tibiotalar dislocations without associated fractures. Clin Orthop 1989;239(Feb):207-210
Dr Tranovich is an orthopedic surgeon at the Wooster Regional Practice of The Cleveland Clinic Foundation in Wooster, Ohio. Address correspondence to Mark Tranovich, MD, The Cleveland Clinic Foundation, Wooster Regional Practice, 721 E Milltown Rd, Wooster, OH 44691; e-mail to mtrano@hotmail.com.
Disclosure information: Dr Tranovich discloses no significant relationship with any manufacturer of any commercial product mentioned in this article. No drug is mentioned in this article for an unlabeled use.
Copyright (C) 2003. The McGraw-Hill Companies. All Rights Reserved
E-mail Privacy Policy